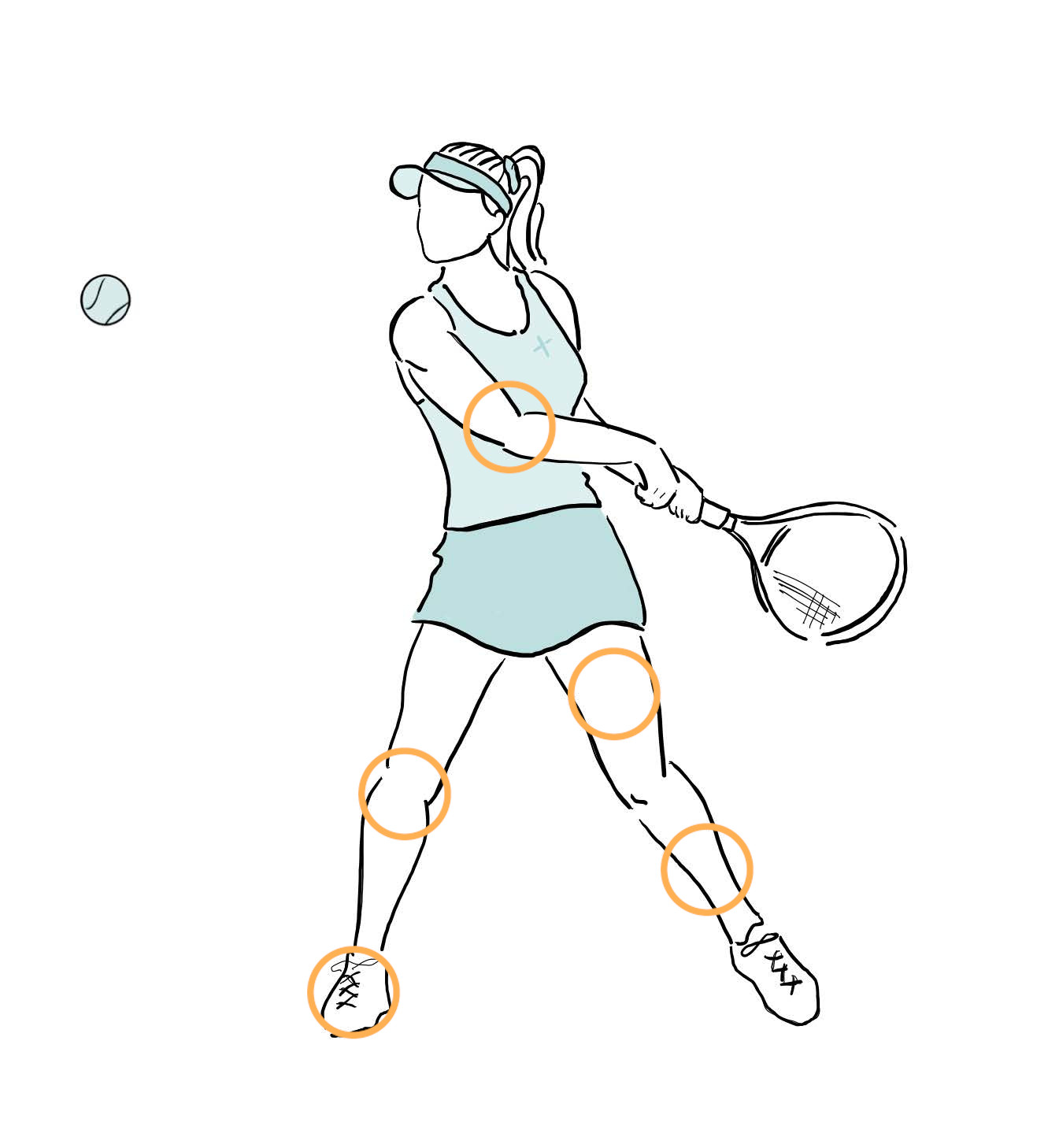
Sports Injury
Knee injuries are common in both amateur and professional sportspeople and the treatment of sporting injuries has undergone significant advancement in recent years.
Surgeons have gone from simply reconstructing ACL injuries and excising damaged menisci to recognising and treating a much larger portfolio of injuries and afflictions.
Dr Stevens brings a modern approach to sport and knee injury and has undertaken subspecialty training in this area at the Avon Orthopaedic Centre in England.
He has particular interest in ACL reconstruction, meniscus surgery, and surgical treatment of unstable or slipping knee caps.
ACL injuries typically occur when a person lands awkwardly or twist their knee excessively such that force of injury tears the ACL.
A knee injury where the ACL is torn may also involve other parts of the knee including the meniscus, bone, joint capsule, collateral ligaments and, in severe cases, the posterior cruciate ligament.
Not all ACL injuries require surgery. Physiotherapy alone can significantly improve knee stability, however, it does not restore the ligament and there is very limited potential for natural healing to occur. Most people wanting to get back to sport and physical activity will need an ACL reconstruction but there are of course exceptions.
Although an isolated ACL injury does not usually require urgent surgery there may be other associated injuries that require urgent attention. It is always best to be seen by a surgeon as soon as possible.
A discussion with Dr Stevens regarding what activities you would like to return to as well as the advantages and risks of surgery will help guide you in making decisions about the treatment of your knee injury
Typically, patients will require physiotherapy before and after surgery.
The value of physiotherapy cannot be overemphasised. The goals of the physiotherapy program are to:
- Enable you to enter surgery with the greatest fitness possible
- Provide you with a knee that has minimal swelling, good range of movement and little pain before the operation
- Avoid postoperative stiffness
- Rehabilitate muscle strength
- Rehabilitate knee co-ordination
- Help you avoid high-risk activities whilst you undertake rehabilitation
- Get you back to the activities you enjoy
Surgical Fact Sheets
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
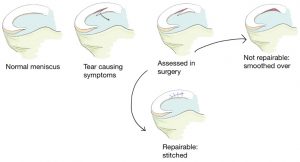
Meniscal Tears
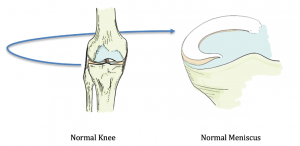
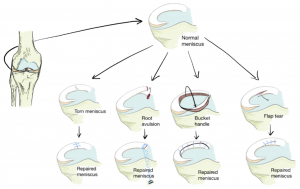
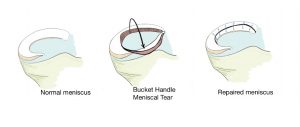
Injuries to the meniscus are common and can occur at any age. He there are two menisci and they act as shock absorbers in the knee – damage to a meniscus can lead to problems within the knee and arthritis.
If the meniscus has been injured through wear and tear with arthritis also being present in the knee then it can be treated without surgery. Physiotherapy, activity modification and pain relief medications can help the symptoms.
Some tears can be serious and require surgery. People with significant tears may experience pain, inability to bend or straighten the knee, pain on walking and may have a limp.

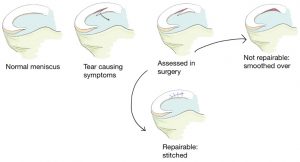
A tear in the meniscus may require surgery. Dr Stevens will assess the movement of the knee and will likely order an MRI scan if this hasn’t been done already.
If the tear can be fixed then surgery to place sutures to hold the meniscus can be performed, usually through keyhole surgery. If the tear cannot be fixed then the torn portion of the meniscus is smoothed through keyhole surgery. Dr Stevens will discuss this with you.
After surgery, you may be able to begin to move the hip, ankle and knee under the instruction of Dr Stevens. Placing weight on the leg will depend on the type meniscal tear surgery you have had and how if the meniscus needed to be fixed. You may require a brace and physiotherapy for the knee once the wounds have healed.
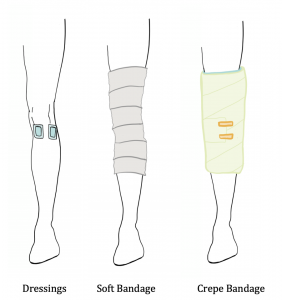
A soft bandage and crepe will be placed over the leg following surgery. As the tissue and bone heal, a small amount of blood may appear on the dressings. This is normal. Sometimes, replacing the bandage is required to reinforce any areas that continue to bleed.

Elevate the leg for the first few days following surgery. You may be placed on blood thinning medications such as aspirin to help reduce the risk of clots.
Discharge home: After your surgery you will stay in hospital overnight and potentially for a few days. You will be discharged with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next week or so as you need. “
Looking after the Bandage: You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee and leg, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot, ankle, knee and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation. You may experience some knee pain in the weeks following surgery. You will need crutches or a frame to walk after surgery. Sometimes the knee may swell in the first 3 weeks. This is normal, but any redness, calf pain or sign of infection should be seen to by a doctor quickly.
It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle movement and walking with your crutches is advised.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review:
After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of surgery to the tibia you have had and the type of work you do. Most surgeries will need 2-6 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with surgery of the meniscus. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Arthritis of the knee may also occur as time goes on as a result of the injury. Sometimes, further surgery is required if more of the meniscus is damaged through injury.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
Meniscal Tears
Discharge home: After your surgery you will stay in recovery until you can sit up and safely begin to move around. When you are comfortable you can be discharged home with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next to take for two to three of days as you need.
Looking after the Bandage: There will be a dressing over the surgical incision on the front of the knee. You will have a white soft bandage and then a crepe bandage over this. This helps to keep compression on the knee as it heals.

You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot ankle and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation. It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle walking and exercise is helpful.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review: After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Physiotherapy: Physiotherapy may be needed to your knee moving and strong again, but do not start this until you have had your appointment with Dr Stevens at 2 weeks.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of meniscal surgery you have had and the type of work you do. Most surgeries will need 2 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with performing surgery on your meniscus. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Injury to the remaining meniscus is a possibility in the future and knee arthritis may occur as a result of the injury.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
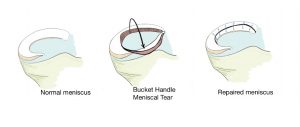
Meniscal Repairs
Injuries to the meniscus are common and can occur at any age. There are two menisci and they act as shock absorbers in the knee – damage to a meniscus can lead to problems within the knee and arthritis.
If the meniscus has been injured through wear and tear with arthritis also being present in the knee, then it can normally be treated without surgery. Physiotherapy, activity modification and pain relief medications can help the symptoms.
Some tears can be serious and require surgery. People with significant tears may experience pain, inability to bend or straighten the knee, pain on walking and may have a limp.
A tear in the meniscus may be repairable through surgery. Dr Stevens will assess the movement of the knee and will likely order an MRI scan if this hasn’t been done already.
If the tear is repairable, then surgery to place stitches to hold the meniscus in place can be performed, usually through keyhole surgery. If the tear cannot be fixed, then the torn portion of the meniscus is smoothed over through keyhole surgery. Dr Stevens will discuss this with you.
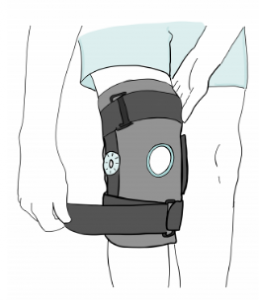
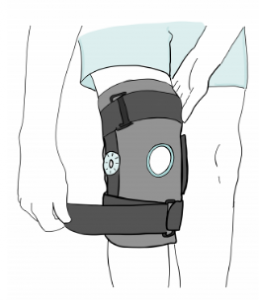
After surgery, you may be able to begin to move the hip, ankle and knee under the instruction of Dr Stevens. Placing weight on the leg will depend on the type meniscal tear surgery you have had and how the meniscus was fixed. You may require a brace and physiotherapy for the knee once the wounds have healed.
A soft bandage and crepe will be placed over the leg following surgery. As the tissue and bone heal, a small amount of blood may appear on the dressings. This is normal. Sometimes, replacing the bandage is required to reinforce any areas that continue to bleed.
Elevate the leg for the first few days following surgery. You may be placed on blood thinning medications such as aspirin to help reduce the risk of clots.
Discharge home: After your surgery you will stay in hospital overnight and potentially for a few days. You will be discharged with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next week or so as you need.
Looking after the Bandage: You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee and leg, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot, ankle, knee and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation. You may experience some knee pain in the weeks following surgery. You will need crutches or a frame to walk after surgery. Sometimes the knee may swell in the first 3 weeks. This is normal, but any redness, calf pain or sign of infection should be seen to by a doctor quickly.
It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle movement and walking with your crutches is advised.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review: After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of surgery to the tibia you have had and the type of work you do. Most surgeries will need 2-6 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with surgery of the meniscus. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Arthritis of the knee may also occur as time goes on as a result of the injury. Sometimes, further surgery is required if more of the meniscus is damaged through injury.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
Looking after your Knee following Meniscal Repair
Discharge home: After your surgery you will stay in recovery until you can sit up and safely begin to move around. When you are comfortable you can be discharged home with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. Meniscal Surgery normally results in the knee being slightly more swollen than other knee operations. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next to take for two or three days as you need.
Looking after the Bandage: There will be a dressing over the surgical incision on the front of the knee. You will have a white soft bandage and then a crepe bandage over this. This helps to keep compression on the knee as it heals.
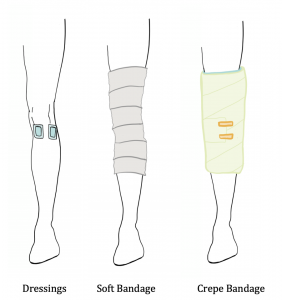
You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot, ankle and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation.
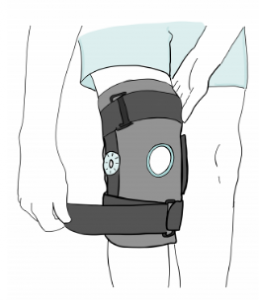
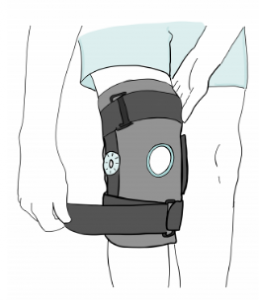
Often a hinged knee brace will be applied to stop the knee bending too much. It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle walking and exercise is helpful.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review: After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Physiotherapy: Physiotherapy may be needed to your knee moving and strong again, but do not start this until you have had your appointment with Dr Stevens at 2 weeks.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of meniscal surgery you have had and the type of work you do. Most surgeries will need 4-6 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with performing surgery on your meniscus. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Further injury to the repaired meniscus is a possibility in the future and knee arthritis may occur as a result of the injury. If further injury occurs, a second repair is not often possible and so an operation to smooth over the torn meniscus may be required.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
ACL Injuries
Injuries to the ACL are common in Australia. They are usually as a result of a twisting injury playing sport but may also occur from an awkward fall, accident or workplace injury. The ACL helps to provide stability to the knee. After an ACL injury you may have pain when walking and the knee may not bend or straighten out fully. It is important that you see a surgeon and physiotherapist soon after the injury to check for other knee conditions.
If you are active, enjoy sport and have instability in the knee following an ACL tear then surgical reconstruction of the knee is often advisable. Non-surgical treatment can be successful and involves a rehabilitation program with dedicated physiotherapists.
Some tears can be serious and can involve damage to other parts of the knee. These may require surgery to reconstruct the ACL and repair the damaged areas of the knee. People with significant ACL tears may experience instability of the knee and swelling.
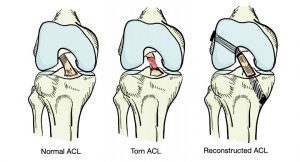
Dr Stevens will assess the movement of the knee and will likely order an MRI scan if this hasn’t been done already. If reconstruction is advisable, then surgery to replace the torn ACL with a graft is organised. The graft can come from several different places and Dr Stevens can discuss the options with you.
If the ACL tear is associated with a meniscal tear, Dr Stevens can discuss fixing the tear by placing sutures in to hold the meniscus in place, usually through keyhole surgery. If the meniscal tear cannot be fixed then the torn portion of the meniscus are smoothed over through keyhole surgery.
What to expect after surgery:
If you and Dr Stevens decide that surgery is the best option for your ACL injury, you will stay in hospital overnight following your surgery. You can be discharged the next day with pain relief -take the pain relief tablets for two to three of days as you need them.
You will have a dressing on your surgery site and a bandage which needs to stay clean and dry for 14 days.
You can move your feet and hip straight away, but the dressing on the knee will prevent it form moving too much.
After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Physiotherapy is strongly encouraged to help the knee move and to regain strength. Do not start this until you have had your appointment with Dr Stevens at 2 weeks.
There are risks with surgery. These include infection, knee pain and stiffness, graft rupture and failure to get back to high end sport. Arthritis may occur in the future as a result of the damage caused by the injury. Dr Stevens will discuss the risks of surgery with you.
ACL Injuries
Discharge home: After your surgery you will stay in hospital overnight and can be discharged the following day with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next to take for two to three of days as you need.
Looking after the Bandage: There will be a dressing over the surgical incision on the front of the knee. You will have a white soft bandage and then a crepe bandage over this. This helps to keep compression on the knee as it heals.

You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot ankle and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation.
It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle walking and exercise is helpful.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review: After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Physiotherapy: Physiotherapy will be needed to your knee moving and strong again, but do not start this until you have had your appointment with Dr Stevens at 2 weeks.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of ACL surgery you have had and the type of work you do. Most surgeries will need 2 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with reconstructing your ACL. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Rupture of the ACL graft is a possibility in the future and knee arthritis may occur as a result of the injury.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
Quadricep Tendon Injuries
The large thigh muscle known as Quadriceps is attached to the knee-cap by an important tendon known as the Quadricep tendon. This can be injured and torn. If this happens, knee surgery is often required.
Dr Stevens will assess your knee and often order an MRI scan to gain information about the injury.
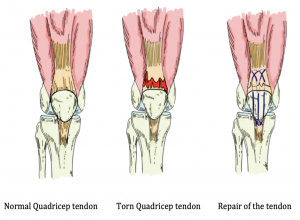
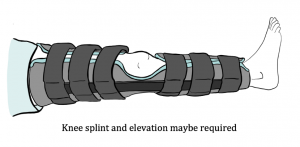
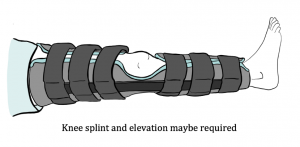
A tear in the Quadricep tendon may require surgery. If the tear can be fixed then surgery to place sutures to hold the tendon in place can be performed. Surgery is normally completed by placing sutures into the tendon and passing them through the knee-cap bone. Prior to surgery you will need a Zimmer knee splint.
Discharge home: After your surgery you will stay in recovery until you can sit up and safely begin to move around. You will need to spend at least one night in hospital. When you are comfortable you can be discharged home with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next to take for two or three days as you need.
Looking after the Bandage: There will be a dressing over the surgical incision on the front of the knee. You will have a white soft bandage and then a crepe bandage over this. This helps to keep compression on the knee as it heals.

You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot, ankle and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation.
Often a hinged knee brace will be applied to stop the knee bending too much. It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle walking and exercise is helpful.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review: After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Physiotherapy: Physiotherapy may be needed to your knee moving and strong again, but do not start this until you have had your appointment with Dr Stevens at 2 weeks.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of work you do. Most surgeries will need 4-6 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with performing surgery on your torn tendon. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Further injury to the repaired tendon is a possibility in the future and knee arthritis may occur as a result of the injury.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
Patella Tendon Injuries
The large thigh muscle known as Quadriceps is attached to the knee-cap by an important tendon known as the Quadricep tendon. The Knee-cap is connected to the lower leg by the patella tendon. This can be injured and torn. If this happens, knee surgery is often required.
Dr Stevens will assess your knee and often order an MRI scan to gain information about the injury.
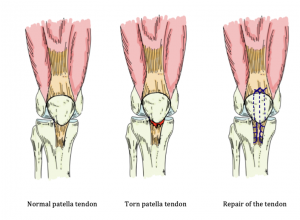
A tear in the Patella tendon may require surgery. If the tear can be fixed then surgery to place sutures to hold the tendon in place can be performed. Surgery is normally completed by placing sutures into the tendon and passing them through the knee-cap bone. Prior to surgery you will need a Zimmer knee splint.
Discharge home: After your surgery you will stay in recovery until you can sit up and safely begin to move around. You will need to spend at least one night in hospital. When you are comfortable you can be discharged home with pain relief tablets.
Pain relief: After surgery it is normal to have some pain or discomfort. The amount of surgery you have had will influence how much pain you can expect and how long you will need pain relief for. You will be given pain relief tablets to take home with you when you leave the hospital. Take these over the next to take for two or three days as you need.
Looking after the Bandage: There will be a dressing over the surgical incision on the front of the knee. You will have a white soft bandage and then a crepe bandage over this. This helps to keep compression on the knee as it heals.

You will need to keep the bandage clean and dry. The Crepe and Soft Bandage can come off when they get loose. You may want to re-wrap your knee, otherwise you can discard these bandages. Keep the dressings that cover your wounds dry for the first 2 weeks.
Movement after surgery: You can move your foot, ankle and hip straight away after surgery. Your knee will slowly be able to bend in the days that follow your operation.
Often a hinged knee brace will be applied to stop the knee bending too much. It is a good idea to keep moving even after your surgery, it helps your blood circulation and stops your body getting too weak. Avoid any strenuous activity for the first 2 weeks, but gentle walking and exercise is helpful.
When you are resting or sleeping try to keep the leg straight and elevated on some pillows.
Wound review: After 2 weeks you will have an appointment with Dr Stevens to have your wound checked, any stitches will be removed. Dr Stevens will then give you advice on exercises and physiotherapy.
Physiotherapy: Physiotherapy may be needed to your knee moving and strong again, but do not start this until you have had your appointment with Dr Stevens at 2 weeks.
Driving: You cannot drive until you have had your first review appointment with Dr Stevens. He will give you an indication then when you are likely to be able to drive again
Returning to work: This depends on the type of work you do. Most surgeries will need 4-6 weeks off work, some will require longer, especially if you have a manual job.
As with all surgery, there are risks with performing surgery on your torn tendon. These include infection, delayed healing or wound problems. Difficulty with pain and range of movement may also be occur. Further injury to the repaired tendon is a possibility in the future and knee arthritis may occur as a result of the injury.
+ Fever
+ Heavy bleeding or ooze from the wound
+ Increased swelling and redness around the surgery site
+ Pain in the calf muscles or difficulty breathing
If you have any of these problems, please call Dr Stevens or his rooms on 03 5752 5020
INTERACTIVE SPORTS INJURY GUIDELINES